(The author is a friend and so is the subject of his epistle, what I call a long, love letter to God. Both are lawyers but that is not what endears them to me. It’s their unshakeable trust in the mercy and unbelievability of God Almighty, which is essayed more than once in this awesome love story. – Abraham de la Torre)
No Heartbeat for 10 minutes
“WAS I REALLY without heart beat for 10 minutes?” This was Marilou’s question written in halting English on a piece of paper. She could not speak as she was intubated. The day before (August 3, 2022), she suffered a seizure on the operating table as she was being prepared for TAVR (Transcatheter aortic valve replacement) in St. Luke’s Medical Center, BGC.
At 6:30 AM of August 4, 2022, long before visiting hours, a nurse from the CCU (Coronary Care Unit, the equivalent of ICU) told me “Your wife is looking for you!” She had scribbled the question, along with many others – mostly written angrily, in quick succession (this was the lawyer cross-examining), appalled that after the seizure the day before, I would agree to go on with the TAVR.
It never dawned on me how serious this statement was – “she had a seizure but we were able to revive her.” Information would trickle in to complete the picture, as doctors were added to her medical team to address issues that had suddenly arisen.
She said her heart cannot possibly take it! I said I am convinced it is her only chance of survival. I cried a river. Her only chance for survival was also, in all selfishness, the only way I can continue to have her in my life. But I was going to respect her decision. Sometime ago, our children and I have decided that, as difficult as the situation that we were in, it was more difficult for her and, if grudgingly, we were going to respect her wishes if she says no to further treatment.
(Marilou: After my seizure, I woke up with tubes on my mouth and nose last Wednesday, August 3, with Noel at my bedside at the CCU. With my eyes doing the talking, I pleaded with him not to push through with the TAVR on Friday because I felt my body could no longer bear the ordeal. But he looked at me tearfully and whispered repeatedly “I’m not yet ready to let you go.” That was it. I decided to continue fighting for him! But we entrusted everything to God. And that He would work through our medical team, our loving family, friends, and communities. When all are united in prayer before God, nothing is impossible! All my doctors say it was a miracle my heart beat again after being dead for 10 minutes. They also did not give up on the CPR.
[Note: Marilou got her timeline wrong. She was groggy all afternoon of August 3; by Wednesday afternoon of the seizure, a decision has not been made on the Friday August 5 TAVR as the Neurologist was still completing his examination. Her note writing took place in the morning of August 4, Thursday; on this day, the Neurologist finally cleared her for TAVR, provided she is allowed to rest the whole day and the coming evening. That “I’m not yet ready to let you go!” was said not repeatedly but once! And it was apparently enough!])
Understanding Marilou’s health issues needs a 20-year look-back.
Permanent Heart Failure
On May 23, 2022, a 2D Echocardiogram showed she her permanent heart failure. The findings this day were compared to an earlier 2d Echo done around 2019. A more frequent schedule was in order but the raging Covid pandemic deprived us of regularity. The salient points are these: a) her aortic stenosis (the narrowing of the aortic valve), previously mild was now severe, constricting blood flow from the heart to the rest of the body; b) her mitral stenosis (the narrowing of the heart’s mitral valve), previously mild was now severe. This abnormality prevents the valve from opening properly, blocking blood flow into the main pumping chamber of the heart (the left ventricle).
As a result, she was having shortness of breath and got tired easily although she was managing it by taking frequent rests. She managed it so well the episodes were practically unobservable by us around her.
I am unable to decide if the hectic and toxic work from home schedule (which forced Marilou too many times to work till the wee hours of the morning) conspired to mask the worsening condition of her heart or if it contributed to making it worse. Marilou’s Cardiologist Dr. Rey (note: all Doctors were referred to using their first names) supplied the answer: it is a major contributor and she should retire. A second Cardiologist, Dr. Lowe, said the same.
Back to the Doctors
Marilou was diligently following regular appointments until the pandemic intervened. So the usual “What brings you here?” always begged for an answer. “I am having shortness of breath, I tire easily.” Here is the explanation: as the pandemic eased up, the 2022 Presidential campaign heated up. Our family was rabidly behind the Leni-Kiko tandem. It was clear Marilou was aching to attend a campaign rally. Most of us have attended but she stayed home because of the danger of Covid exposure; of course, she did not tell us she would get tired.
But she just had to go, and off we went to the rally in Pasay City on April 24, 2022, Leni’s birthday. We walked from our HQ at Century Park Hotel on Vito Cruz and stayed the whole time, from 5 PM until around 10 PM when it ended.
She was caught in the crush of rallyists leaving for home. Deprived of her pacing which was a trick to manage her tiredness and shortness of breath, she nearly fainted midway through a pedestrian overpass. Angels swooped in, offering water, food comfort, a hand-held battery-operated fan that was left with her. She regained her bearing but we understood much later it could have been a terminal attack she avoided.
So, off we went to her Cardiologist Dr. Rey, who wrote a prescription for 2d Echo. The line was long and we got a schedule for May 23, 2022. The result of this 2d Echo shattered all the “normalcy” we felt after the major improvement of her heart following her 2017 bypass surgery.
The Bypass Surgery
In August 2017, Marilou had a heart attack at home. It was a slow developing one. I continue to believe so because she started feeling unwell the night before (a Friday, the 4th of August) and it was already Saturday morning of the 5th of August (oh, August again! And how these dates in 2017 and 2022 coincide!) when Bianca and I took her to the St. Luke’s ER (ERod) on the advice of Dr. Clare, who made an early home visit, to at least get an ECG.
Marilou did not want to call Dr. Rey; she knew what he would tell her. On the way, I would call Dr. Lorna, a St. Luke’s doctor, who called ER to tell them we were coming in and it is most likely a heart attack. So the ER was prepared with a team for that, skipping the usual preliminary interview.
Blood was drawn and tested as a first step and immediately revealed high levels of troponin in her blood. (Troponin is in the heart muscles but not in the blood. The heart sends it out to the blood to signal damage to the heart. When the damage to the heart increases, more troponin is released to the blood.)
Months before, Marilou was having episodes of tiredness and shortness of breath. Long walks would tire her. Eventually, the tiredness came even on short walks. At that time, she did not have a regular Cardiologist. The first we consulted said she needs an angiogram. She hoped to find a doctor who would not tell us that “she needs an angiogram.” We were a balikbayan of sorts to Dr. Rey as we had been his patients for his Internal Medicine expertise. Marilou had always liked him, his ways, his manners.
But Dr. Rey also said she needed an angiogram. Marilou was adamant she did not want to get one. Eventually, he convinced her to take a CTA (Computed Tomography Angiography) at least and, since it was just a scan, she relented. The results confirmed she had numerous blockages in her coronary arteries but the CTA only gave 2d views and did not show how narrow the blockages were. Only an angiogram would show these in 3D but Marilou continued to refuse to have one.
But now, with a heart attack, Dr. Rey managed to convince Marilou to get an angiogram – and, if necessary, an angioplasty in the same setup. She relented.
Unfortunately, the angiogram would show that what Marilou needed was a bypass surgery (CABG – Coronary Artery Bypass Graft).
Marilou’s Cancer History
Nineteen years prior to the 2017 episode, in May 1998, Marilou was diagnosed with breast cancer. In the 2 years that followed, she would be stage 4 twice, the second in 1999 metastatic to the bones in 3 areas according to the bone scan which was prescribed following Marilou’s tremendous back pains. The pain came from those affected bones. Her Oncologist, Dr. Trixie, told me to prepare for palliative care which, she said, will last for five (5) months, perhaps shorter.
She had undergone 3 chemotherapy sessions using various drugs. The second chemotherapy was after the 1st metastasis in an aggressive treatment in the US (MD Anderson Cancer Center in Houston, Texas) using the much-touted wonder drug Herceptin combined with an old chemo drug. Herceptin was newly approved and the hospital was testing its efficacy in combination with old chemo drugs.
We were warned of the possible effect to the heart, which will grow older faster (by as much as 10 years, Dr. Vicente, her US doctor said) than her body. But cancer was the enemy at that time. The heart was scanned monthly to determine the ejection fraction, but concern for that side effect took a back seat.
She also had radiation after her first round of chemotherapy treatment. This cancer history made the team assembled by Dr. Rey balk at bypass surgery. Dr. Estan had seen patients with the same history in an “open and close” situation – meaning, heart showed it was beyond help even through bypass surgery. After oncologist Dr. Charity cleared Marilou from any metastasis, and aware of the risks that the past cancer treatment may yet show the heart and the arteries unavailable for bypass surgery, we gave the team our consent for CABG.
Marilou had 8 blockages in her arteries. Four were in 2 arteries that were bypassed. Four blockages remained. I understood that cancer treatment made these blockages impossible for bypass. Dr. Rey said we leave these to God’s work!
By that time, tests already showed aortic and mitral valves problem, although with Marilou’s condition at that time, their replacement at the same time as the bypass surgery would have been too precarious. First, she had to live. To fight another day.
Nevertheless, Marilou’s heart greatly improved. She would pass strings of stress tests and then our lives slid into lethargy with the onset of the Covid pandemic.
Open-Heart Surgery Part 2
As shown by the May 2022 2d Echo, the aortic and mitral valves problem worsened. In theory, the only way to address both at the same time is through an open-heart surgery. But several doctors we consulted would not recommend it based on – again – Marilou’s health condition. One in particular, Dr. Jorge, also said addressing the aortic valve problem could solve the mitral valve problem – or at the very least delay its progression. All say leave the mitral valve problem to prayers!
Enter TAVR
Doctors Jorge, Estan, and Rey all recommended TAVR. Dr. Lowe talked about it.
In 2017, Marilou’s medical team said that if the aortic valve acts up, TAVR is a very good option. I read on it immediately – and found that there is one, Dr. Enrique, who was the acknowledged pioneer of this procedure in the Philippines. By a mile, the doctors say now, he leads in a number of procedures undertaken and, more importantly, in success rate.
The first TAVR procedure was performed on April 16, 2002 in Rouen, France. We consulted Dr. Enrique and he laid out the plans including preliminary CT SCAN and assembling a medical team which, given Marilou’s health condition (there we go again!), would have an open-heart surgery team in case one is needed in an emergency.
CT Scan confirmed Marilou was a good candidate for TAVR. We checked into the hospital on Friday, July 29, for the first procedure, an angiogram, on Saturday July 30. The angiogram showed Marilou’s 2017 bypass grafts are in very good condition. It also showed that the left main (left main coronary artery – LMCA) where oxygenated blood arrives from the lungs before the heart pumps it out to the rest of the body could receive a stent after the aortic valve is replaced. This left main was already bypassed in 2017 but to simplify, the catheter/probe will be so close that it is a good opportunity to address that left main problem which is 100% blocked.
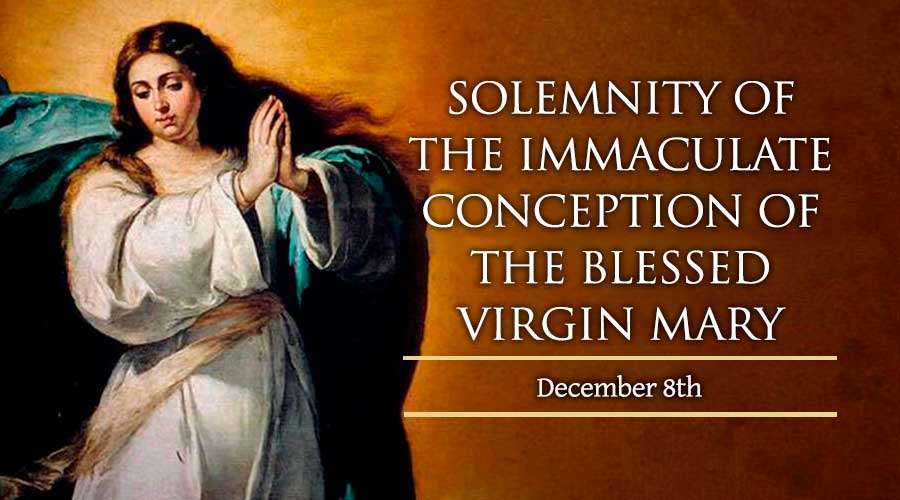
It’s like travelling to Baguio or coming home from there. Manaoag is so near but requires a short detour. Even if that is not the main purpose of your trip, why not pass by Our Lady of Manaoag Church to thank our Mother Mary for her constant protection? Incidentally, before we saw Dr. Enrique for the first time, we visited Manaoag to ask for our Mother’s help.
Dr. Enrique said the stent on the left main will greatly help the 2017 bypass and the hope is it addresses as well the mitral problem. So it was decided there will be a TAVR and angioplasty at the same time.
Prayerful Doctors and Prayer Warriors
The medical terms and procedures are mostly alien to us – we are both lawyers, after all, and we needed to place full trust on our doctors, especially on how the procedures are undertaken, how they work, and the benefits that are derivable from them. It helps greatly that this trust is placed on God-fearing people.
Dr. Enrique told us to pray for the success of the procedure – and for the doctors as well. This is at least not strange. Dr. Rey has always been prayerful. And so is Dr. Estan, we know, and Marilou is with his group as Cooperator. Dr. Remy, too, who was Marilou’s Infectious Disease doctor during her 2017 bypass (when Marilou had a hospital-acquired pneumonia!), has been in service of the Church for a long time. From as early as Marilou’s cancer doctors (even in the US), everyone believed in the power of prayer and how God makes everything possible.
So we asked our prayer warriors to include them in their prayers. Our praying community has multiplied since Marilou’s cancer treatment. We can say this surely is one good side/truth of an ailing social media network full of fake news and false hopes. Our praying community has even become international.
I for one prayed – “Lord, these are skills You yourself showered on these doctors; it was You Lord, who made the invention of this procedure possible, You are our heavenly doctor, and so we ask Lord that this be safe, successful, and without complications. And make the doctors bring their A-game to this procedure.”
Prayers intensified as demanded by circumstances and as a result of my frequent updates. There was no let-up.
God Intervenes
Doesn’t He? And always? And He even made Himself obvious in so many ways.
Our original date for TAVR was August 1, Monday. When Dr. Enrique visited our hospital room on July 30, after the angiogram, he said August 2. The first delay – the cause was not explained to us.
But on August 2, minutes after she was wheeled into the Cath Lab (Catherization Laboratory) – the equivalent of the operating room – I was informed Dr. Enrique decided to postpone the surgery until after the nature of the antibody found in Marilou’s blood drawn the night before is determined. It seemed there is danger that the antibody would rebel against the blood the hospital had in storage (in case there is need for transfusion) which did not have the same antibody. Back to the hospital room, after just an hour, the Hematologist, a new member of the team, visited to tell us the antibody (technical term forgotten) is, in short, a “nuisance antibody” and not capable of any defensive role, or as its name implies – a “nuisance.” But it was too late to call back the medical team.
The Seizure in the Cath Lab
Our next date was set – Wednesday, August 3, 1 PM. But at 9 AM, we were told the procedure was moved to 11 AM. At 9:30 AM, Marilou was taken to the Cath Lab. Dr. Enrique was even joking, holding what looked like a pandesal as she told Marilou he was having breakfast for her because she was fasting.
I was in the waiting room. I was the only one there. I knew from conversations among hospital staff which I overheard that Marilou’s procedure was the only one on their schedule. They reveled at the hope of a slow day and early dismissal! So when there suddenly was a frantic activity around me, I suspected correctly something was amiss.
After just 30 minutes into the inner Cath Lab, Dr. Enrique called me. Heart pounding, I just heard – “she had a seizure, we revived her after 12 minutes.” I asked questions and from answers given, these were what I gathered at that point:
- They were still preparing Marilou for the procedure when the seizure started.
- They revived her after 12 minutes.
- If this had been in the hospital room, she would not have survived. (In hindsight, the seizure was looming and God – who else? – was delaying everything so it did not come midstream into the procedure. Even the antibody was there not really as a nuisance but a great factor in delaying the procedure. But Wednesday, God also advanced the time so that Marilou does not suffer from heart attack in the hospital room.)
- That she was in the Cath lab and not elsewhere was instrumental to her survival. The team was in place, the best that can be gathered for that TAVR, and she was not even for a moment unattended. They did CPR immediately.
- But they’d have to get a Neurologist into the team to determine the condition of the brain and to rule out the seizure was from it.
- “This is how they die!” Meaning, Dr. Enrique said, patients with aortic stenosis die this way, just too suddenly.
The walking time bomb now had a face. With just one IV bag and one IV flow rate regulator when she was wheeled into the Cath Lab, Marilou came out of it intubated, tube onto the nose for feeding, an external pacemaker, with numerous IV bags converging into the 4 IV flow rate regulators. It was a scene right out of the Korean telenovelas Marilou had been following. One look and you know she was in bad shape.
She was taken to the CCU nearby heavily sedated.
As she slept, we would talk to Dr. Enrique and Dr. Ludwig (the Neurologist) various times. Right after the seizure, Marilou was assessed by a Neurologist to be a 3 in a scale of 1-10, 10 being the highest. In an emergency, the bare minimum would be a 5.
There were also new doctors and, because of her intubation, a Pulmonologist, long-time friend Dr. Ruth was taken on board. Dr. Enrique was adamant the TAVR had to go through as the only one that could guarantee her survival. But of course, we needed to give our consent to it. That consent and the opinion of the Neurologist who was still conducting various tests stood in the way.
The day after the seizure, I asked our good friend Fr. Jigs to give her anew the Sacrament of Anointing the sick (the earlier anointing was just 2 months away when we got the “permanent heart failure” diagnosis). The anointer cried at the pitiful site of the anointee and was still in tears outside. (Bianca: I thought Fr. Jigs would be unable to finish the rites.)
The Written Questions
So back to where we started this piece. The morning after the August 3 seizure. The question “Was I really without heart beat for 10 minutes?” was followed by frantic writing on bond papers on a clip board. With both hands tied to the bed, a cautionary measure to prevent her from pulling out tubes, writing for her was difficult. The lawyer was writing like a doctor! I could not follow, unable to read what was being written. She was losing patience. But reading was difficult until I found out that if I followed what she was writing letter by letter, it was easier to decipher. The punctuation marks were forceful. Essentially: Why did you agree? My heart can’t take it! I will die! I don’t like this tube. Have it removed. Talk to Ruth. She said I don’t need it.
She was angry. Scolding a nurse.
Why am I tied to the bed? What’s this tube on my nose?
There was clear urgency to her questions. But I think these were questions that showed she was back, wanting to regain control of her life. She was feisty! And I was at the receiving end. It was familiar territory for both of us.
These questions would be repeated to Dr. Enrique. I have answered the questions as best as I could, based on conversations with the doctors, but I told Dr. Enrique she won’t listen except to him.
Why go on with the TAVR? – “We believe it’s your only chance of survival. With that seizure yesterday, this TAVR is key.”
Remove this tube. – “You don’t need it now, you are breathing on your own, but we want to keep it in case we need it, rather than labor through reinserting it at the point when we need it.”
Why am I tied to the bed? – “We don’t want you removing your tubes but if you promise you will not pull them out, I will remove them myself. We have a deal?” (She nodded and was liberated.)
Eventually, she would agree to do the TAVR. And the Neuro Dr. Ludwig gave his go-signal. Just a day after the seizure, he found Marilou’s recovery remarkable. Dr. Enrique told me Marilou was in better shape for the TAVR than before her seizure.
TAVR Day
Days before, Bianca, our daughter/4th year medical student in St. Luke’s, was pleading with me to ask Dr. Enrique to let her into the Cath Lab to watch the procedure. I did not dare. I was thinking “This is your mother and bring your medical student’s curiosity elsewhere.” Even if I realized this was a singular chance for her to see the real action of this not-so regular procedure.
TAVR day was August 5, Friday, and at about 7:30 AM, after Marilou was taken from the CCU to the Cath Lab, we chanced upon Dr. Enrique along the corridor, just in front of the waiting room. He asked us to pray for a safe and successful procedure and left us. A few steps later, he turned around and, pointing to Bianca, asked if she wanted in to observe. Bianca of course said yes and ran to look for scrubs.
Bianca’s Account:
Even though I had only a month’s experience of being a clinical clerk, the routine of entering the procedure was already so familiar to me, thanks to my 2-week rotation under Anesthesiology. Change into scrubs, wear a hair cap, put on booties over my shoes. I knew these steps by heart, and yet my hands were shaking as I was in the changing room.
In retrospect, it was probably due to excitement, because not every medical student at my level would be granted the opportunity to observe a procedure like this. It could also have been nerves, since the patient was my Mom, after all.
I had hoped that I would be given a chance to say hello to her, to assure her that she had family in the room, but by the time that Dr. Enrique led me to where the procedure was to take place, she had already been injected with the anesthetic drugs to put her to sleep. As I stood nearby while Dr. Enrique was giving a mini lecture to the Fellows present, I could only watch from a distance as the nurses carried out the rest of the preparations.
Some minutes after we finally entered the operating room, one of the doctors announced that it was time for prayer. When the room fell silent as the leader prayed aloud, I deduced that this was part of their routine. It put me at ease, and I thought to myself that it would have comforted Mom as well, had she been awake to witness it.
Before Dr. Enrique began, he called me to stand behind him where I could have a good view of the giant screen that displayed the X-ray images that guided him through the minimally invasive procedure. I wanted to be a diligent student and maximize the learnings, but during that moment, I was, first and foremost, the daughter of the patient on the table.
So I prayed, as Mom would have wanted.
And I tried my best not to “freak out,” as was the condition of Dr. Enrique when he allowed me to observe.
The Two Nurses on the Corridor
After just one hour, at a little past 9 AM, as I was pacing on the corridor praying the Rosary, two nurses came out of the Cath Lab waiting room. They were on a break, obviously. As they saw me, the one sent by Ate Marie on the day of Marilou’s seizure to check my blood pressure (found to be elevated) smiled at me and said, “Sir, it’s done. Go inside already as Dr. Enrique should be calling you anytime now.” All this time, she was smiling. To me, this was like saying “It was successful!”
True enough, as Patty and I were about to pull the door, it opened and another nurse told us Dr. Enrique was looking for me.
I expected this procedure to last 2-3 hours. That was what I was told. If I had not seen those two nurses spoiling the good news, getting called by Dr. Enrique after just one hour would have led me to a grand collapse.
An Almost Uneventful TAVR
So, Dr. Enrique told me the good news. One aortic valve and one stent on the left main successfully deployed and both working very well. Even the mitral regurgitation is very subdued (fueling the hope that solving the aortic problem will make the mitral problem go away or, at the very least, no longer as pesky and threatening). Bianca was behind Dr. Enrique, crying. Tears of joy! Sobbing Patty and tearing-up Moy were behind me. It was uneventful but very successful although they had to help Marilou’s heart come up to speed with a short bout of chest compressions.
All this time, Stan was left in the bigger waiting room to tend to our belongings. He slept in the waiting room, first accompanying me, then accompanying Patty the next night when I went home. Barangay Tamase had been occupying half of the waiting room – our home for 4 days. This has been the longest I had been with the children in one room. Ever! Or, at least, in recent memory. An even bigger barangay had the other half. Their patient had a steady stream of visitors. Our would-be visitors are somewhere, in the Church, or at home, praying.
Brian was asleep gathering strength for a trip to the airport. With what has been happening, it was difficult to get sleep at night. So we made do with shorts naps here and there. And Paolo was on the plane about 3 hours away from home in the US.
Later, I found Patty, Bianca, and Moy in deep embrace, still crying.
The Happy Dance and the Ovation
Bianca: “That is one beautiful valve,” Dr. Enrique said when he was looking at the images on the screen. It felt like I was holding my breath (and my tears) during the entire procedure, an effort to keep my promise to Dr. Enrique and to remain professional in the tense operating room. When the doctors and nurses in the room started applauding after his declaration, I finally let a few tears slip. And when Dr. Enrique started happy dancing in place, I couldn’t help but laugh. I was speechless, watching him celebrate like that when he was so serious and commanding during the procedure, mere minutes ago. He turned to give me a thumbs up of reassurance, and when he directed his eyes back at the screen, a great realization started to sink in – what I had just witnessed in the last hour or so was God’s work done through the hands of his servants: Mom’s doctors and nurses.
The Culmination of Everyone’s Prayers
“On our way out of the operating room to talk to Dad, Dr. Enrique asked one of the doctors present to show me Mom’s new echocardiogram results. Recalling what I had seen prior to the procedure, even my novice eyes could tell the difference.
Compared to how it functioned before, it was as if Mom had a new heart now.
Beautiful, Just Beautiful
At the CCU (when Dr. Enrique visited, he would drop by the waiting room and call me/us to go with him even), Dr. Enrique listened to Marilou’s heart with his stethoscope. “Beautiful” he said, “just beautiful.” He did a little happy dance, showing us though so briefly how he danced at the Cath Lab. “But it was a longer dance there.” he said.
Later that same afternoon, the intubation ended (and with it the feeding tube). We were happily surprised to see these new milestones at the next visiting time. It was a promise promptly delivered by Dr. Ruth.
Slowly, the IVs were removed, the pacemaker was removed, Dr. Enrique actually doing the removing or directing – as if there was an all-too-familiar snarl of vehicles needing to be untangled! And Marilou was starting to look like she has always been: “beautiful, just beautiful” I thought.
In the evening, Marilou sat on a Lazy Boy. The following morning, she had breakfast from that Lazy Boy.
Back in the Regular Room
In the evening of the day after the TAVR, we were back in the regular room. The following day, Dr. Enrique asked me to listen to Marilou’s heart through his stethoscope. “Listen to how beautiful it sounds. Sayang, you should have listened to it when I asked you before so you’d know the difference.” After listening, he asked if I heard the heart beat. I said no (but I did!) and told him I just heard it say “I love you, Noel. I love you, Noel.” He had a good laugh.
Miracles and Jubilation
“Wow” has always been a word commonly used to express surprise or awe at positive news. There will be double and triple wows. With each update of progress that came unexpectedly earlier than anticipated, there was instant jubilation. Just as the requests for more prayers were met instantaneously. The faithful understand how God has blessed us with another miracle. Ate Liza said “It’s her second life!” It’s actually the third, maybe even more, because of her cancer, the stage 4 bouts, the 2017 bypass, and now this. Ate Irene would say later Marilou is like a cat with many lives. Surely, God’s faithful daughter who is blessed tremendously.
Not only were our cheerleaders/prayer warriors jubilant. The doctors were, as well. Dr. Marvin said “Wow ! you’ve been through a lot and to see you like this is nothing short of a miracle.” He was there during the seizure as he was the emergency cardiac surgeon. That encapsulates the happiness of Marilou’s victorious medical team. Dr. Enrique would say “We know family is happiest. But doctors are happy, too, not just professionally but also personally. We are friends now.”
Statistically, Marilou is Dr. Enrique’s TAVR Patient No. 211. Just three days after the procedure, Marilou was sent home, punctuating the success of the TAVR and her recovery from it all. There will be aches at home, the effect of the CPR mostly.
Marilou: I feel like I came from a boxing match!
PS – the First Check-up
Marilou had been looking for her shortness of breath. She couldn’t find it!
Dr. Enrique ordered a 2D echo and Marilou had one on August 19. His secretaries told us that after the seizure, Dr. Enrique asked them to pray hard for Marilou. Dr. Enrique would tell us he even asked his wife to pray (he can’t remember the last time he asked for prayers for a patient) and she wondered. He just said – this is a difficult case.
We picked up the results on August 22 and took it to him who pointed out how Marilou’s numbers have improved. But, he said, the heart had seen so much trouble in the past we must go on medicating to let it recover. We will see him in a month – around September 22.
In the meantime, we have a physical rehab to complete and, thereafter, go visit Mama in Cebu. At 94 years old, she’s having her own health troubles. And our Mama in Manaoag is waiting for our “thank-you trip.”